Benefits
Employers Turning to Pharmacy Benefit Managers to Fight Employees’ Prescription Drug Abuse
By Michael A. Perry
Jan. 17, 2020
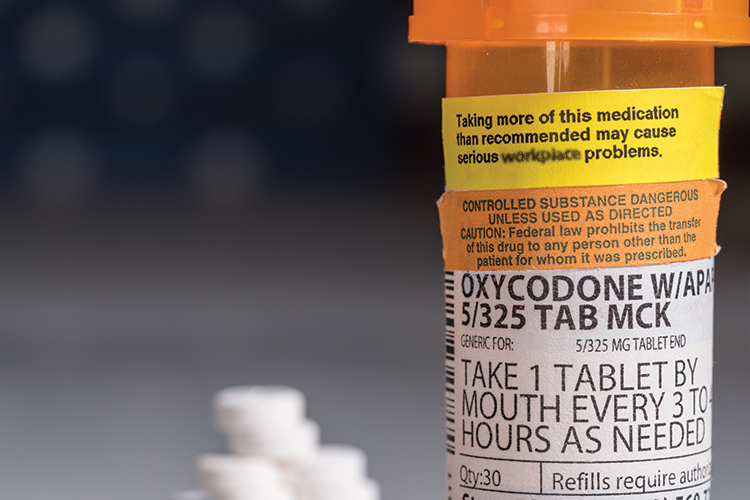
More than 10 million people in the United States misused a prescription opioid in 2018, and the opioid epidemic cost the country $179 billion including mortality, health care expenses, lost productivity, criminal justice expenses and assistance. The National Safety Council notes that the annual direct health care costs of individuals who misuse opioids are 8.7 times higher than those who do not.
The opioid epidemic offers an example of a preventable, complex public health and safety issue that has arisen due to a perfect storm of causative factors. Consequently, it requires multiple stakeholders to develop and deliver an effective solution to help lower costs and improve patient health outcomes. These stakeholders include health care providers, pharmacies, drug manufacturers and even employers.
However, the pharmacy benefit manager is one player in the opioid crisis that fills a critical role by employing clinical programs to ensure safe and appropriate utilization of medications. The PBM is a third-party administrator of prescription drug programs and primarily responsible for contracting with pharmacies for network services, negotiating discounts and rebates with drug manufacturers, developing and maintaining the plan’s list of covered drugs (a formulary), and processing and paying prescription drug claims.
PBMs have become an increasingly important part of health benefits since they first entered the market in the 1970s. Today, three pharmacy benefit managers control more than 80 percent of the American market. All are part of massive health care conglomerates that have interests in other aspects of the benefits food chain — from retail pharmacies to medical insurance.
This can create conflicts of interest, as these mega-corporations stand to profit from every stop on a patient’s journey. These conflicts of interest can in turn leave employers and patients vulnerable to increasing health care costs and crises such as the opioid epidemic.
The American public, from the employee to the executive suite and human resources professionals, as well as those who make decisions about employee-sponsored health care, seeks change in today’s profit-driven benefits industry. Here are just a few of the reasons why:
• In 2017, the average annual cost for prescription drugs used to treat chronic conditions reached $20,000, and drug prices increased at twice the rate of inflation.
• American families spent 67 percent more on health care in 2018 compared to 2008.
• Employer contributions toward health care costs rose 51 percent in the same period.
• More than 66 percent of bankruptcies are due to medical expenses or time out of work as a result of illness.
Mergers and acquisitions may answer the health care industry’s need to create new sources of revenue, but they can leave patients and plan sponsors behind. In a sector dominated by an outsized few, consumers all begin to look the same.
To compound the issue, PBM operations are often seen as veiled enterprises. Complex contracts and opaque business practices conceal the flow of dollars, making it difficult for plan sponsors, HR professionals and members to see what they’re paying for. It may seem impossible to demand meaningful change from such a sizable arm of the health care industry, but it doesn’t have to be.
Human resource professionals occupy a unique position in the U.S. workforce. As part of the decision-making process when it comes to employee benefits, HR leaders can demand change from the industry by learning how to spot PBMs that put member and plan sponsor interests first and move away from PBMs that don’t.
This requires understanding today’s health care landscape and how PBMs should be transforming to work for employers, not just for themselves. Here are four key indicators that demonstrate a PBM has broken from the status quo to operate in the best interests of its clients and their members:
• Pay-for-performance business model.
• Comprehensive clinical programs.
• Complete care coordination.
• Transparent contracting.
Pay for Performance
Most PBMs today operate on a fee-for-service model in which they are paid each time they perform a given function, such as a prior authorization review. While this type of business model is common, it fails to tie the PBM’s financial success to how well the company performs for consumers.
No matter how well or poorly the PBM helps the plan sponsor manage prescription spend, the PBM is paid the same. In some cases, it may even be paid more if the plan’s prescription spending grows based on profit incentives tied to per-claim fees and hidden revenue streams.
That’s why a pay-for-performance business model has so much potential in the PBM industry. Pay for performance is a relatively new model, so far only explored by a few PBMs despite its power to help tie the companies’ interests more closely to those of members and plan sponsors.
The pay-for-performance model helps to support transparent PBM operations by holding PBMs responsible for the quality of the work they do and putting dollars at risk if a plan sponsor’s prescription spending rises above a guaranteed maximum. This puts skin in the game and places people, not profits, first.
Under this type of pay-for-performance structure, the PBM is held accountable. Its success is tied directly to quality of service and whether it reduces overall drug spending through proactive clinical programs that help reduce inappropriate utilization. The plan sponsor is rewarded by performance guarantees tied directly to the PBM’s clinical programs and how well they improve health outcomes and lower costs over time.
This new approach helps encourage a straightforward pricing structure that does not benefit from unnecessary prescribing practices. It eliminates conflicts of interest and places plan sponsors and their members first.
Comprehensive Clinical Programs
Clinical programs can be easily overlooked when it comes to their importance not only in safeguarding patient health, but also in the amount patients and plan sponsors pay for health care each year. While many see programs such as step therapy and clinical reviews for prior authorization as sources of member disruption — and they can be if handled poorly — it’s important to recognize that these programs can positively impact plan sponsors and members alike.
An estimated 40 percent of opioid overdose deaths in 2016 involved a prescription opioid, highlighting the dangers that clinical programs have the chance to prevent. From 2011 to 2016, prescriptions were written for dozens of opioid tablets following surgeries, even when procedures would cause relatively little pain.
This prescribing pattern has tremendous impact, as the probability of long-term opioid use and abuse increases sharply in the early days of therapy, particularly after five days. To prevent addiction and abuse, it is vitally important to ensure patients take prescription opioids no longer than is medically necessary.
PBMs can help to reduce unnecessary opioid prescribing by improving coordination of care among physicians, pharmacists and patients to identify when the potential benefits of these medications outweigh the risks. Comprehensive clinical programs offer a strategic way to ensure medical necessity while protecting patients.
Data from the Centers for Disease Control and Prevention show that the rate of opioid addiction is relatively low if only one day of opioid therapy is prescribed initially, with just 6 percent of patients on opioids one year later. The likelihood of addiction increases sharply with eight or more days of prescription opioid therapy (13.5 percent of patients on opioids one year later). This data demonstrate just one way that clinical programs, such as starter dose and quantity limits, can help protect patients.
Starter dose programs limit the initial supply of a drug to help determine its appropriateness for the patient. In the case of opioids, my company, BeneCard PBF, found that a program limiting the initial supply to three days helped curb the number of prescription opioid claims by 67 percent as part of a comprehensive, clinically driven approach preventing opioid addiction. The starter dose program helps avoid members having excess opioids on hand when therapy is needed for just a few days. This approach also reduces the risk of opioid fraud, waste and abuse.
Quantity limits, which control how much of a medication can be dispensed at a time based on medical best practices, can provide similar protection. This helps to prevent unused medication from building up in the home, where it presents a danger not only to the patient, but to others who may be accidentally exposed to the drug (such as children and pets) or who may be at risk of using the medication without a prescription and a physician’s oversight.
Carefully designed and managed clinical programs have the power to save lives and to protect members and their employers from fraud, waste and abuse of prescription medications. There is an urgent need to do so that extends beyond controlled substance abuse. The United States spends about $21 billion on medication errors and $935 billion in overall health care waste each year. However, many PBMs rely primarily on retrospective reviews of prescription drug utilization to identify problems. This approach may represent a conflict of interest, as many PBMs charge a per-claim fee, meaning they get paid every time a prescription is filled.
Instead, look for a PBM that offers comprehensive clinical programs designed to be proactive, not reactive. These programs should include a retrospective review, but they should also work to identify potential concerns before a medication is dispensed and prevent potentially dangerous or wasteful prescription utilization instead of addressing it after the fact.
Complete Care Coordination
Since today’s health care system is so complex, a clinically driven PBM model is important in protecting patient and plan sponsor interests and helping to control prescription spending.
Unfortunately, many PBMs rely primarily on rebates and negotiated discounts to control prescription spending. While these negotiations are necessary in today’s marketplace, they focus on only one part of the equation.
As in any other industry, obtaining strong discounts is simply not enough. PBMs must also be smart about where and how money is spent. That’s why a clinical focus is key. Rebates and discounts do little good if the number of prescription claims continues to rise because patient welfare has become secondary to numbers on a spreadsheet.
But how do you put people first in this challenging environment? Select a PBM that empowers its pharmacists to coordinate care between the various members of a patient’s health care team. This team can include primary care physicians, specialists, retail pharmacists and others.
Often, these individuals are spread across multiple practices, and communication between them can be difficult. However, the PBM’s pharmacists have a unique perspective, with insight into the prescriptions written and filled by multiple providers. This puts them in an ideal position to facilitate more effective communications between all parties involved in a patient’s care.
PBMs should understand a patient’s condition, symptoms, medical history and any other medications they use to help ensure each prescription dispensed is medically appropriate. They must know each drug’s manufacturer recommendations and FDA guidelines to understand if it offers the most effective course of treatment for that particular individual. PBMs also must take into account industry best practices, which constantly evolve as new medications and new clinical data become available.
All of this helps to support better health outcomes by reducing the risk of side effects and adverse drug reactions, improving treatment efficacy and supporting a better quality of life. This, in turn, can reduce the need for repeat visits to the doctor and lower the risk of hospitalization. It can also lower the risk of patients taking a medication that offers little or no benefit. All of this helps to lower overall health care costs, improve member satisfaction and support a stronger workforce.
Health care must be a coordinated team effort to achieve positive results for both the patients and the PBM.
Transparent Contracting
The ongoing conversation regarding PBMs and their role in controlling costs often focuses on transparency, and it must continue to do so. In many cases, PBMs practice selective transparency, allowing consumers to see only what’s favorable to the PBM and its revenue streams.
Complicated contracts help to conceal revenue streams in an industry where conflicts of interest have become increasingly common. This creates an environment in which human resource professionals and their companies are not fully informed regarding how their money is being spent and where PBMs may be profiting at consumers’ expense.
Convoluted business practices and hidden revenue streams make accurate PBM comparisons virtually impossible. This means that there is a greater chance companies and their employees could be spending more to get less from their PBM.
The traditional PBM business model masks several revenue streams, including rebates and spread pricing, which pharmacy benefit managers enjoy at the expense of plan sponsors and members. To avoid these and other conflicts, it is vital to select a PBM that offers clear contract terms.
Clinically driven pharmacy benefit management works, and because it works so well, there’s no need for complicated contracts that conceal exactly what the plan sponsor and their members are paying for. Another method of avoiding hidden revenue streams and conflicts of interest is to work with an independent or privately owned PBM not beholden to shareholders and not driven by the needs of larger health care ventures. This allows the PBM to focus closely on providing superior service with less emphasis on profit margins. Typically, working with these PBMs means carving out the pharmacy benefit from the medical benefit, which offers further advantages and transparency.
There are several small to midsize privately held PBMs that are advancing clinical care, transparency and innovation — outperforming the industry giants for customer satisfaction in numerous categories. The PBMI “PBM Customer Satisfaction Report” is an annual survey of pharmacy benefit managers’ customers to show client satisfaction in multiple categories such as delivery of promised savings; meets financial guarantees; effective tools to manage prescription costs; no conflicts of interest issues; and other important factors.
Let the Past Inform Our Future
To effectively manage a benefits program and protect its members as well as its financial viability, it is essential to understand the issues inherent in the pharmacy benefit management system, as well as the steps necessary to create meaningful and lasting change. This entails exploring smarter, more strategic PBM clinical programs designed to promote clinical efficacy and reduce wasteful and inappropriate prescription utilization. It also involves resisting the traditional per-claim fee structure, which can be prone to fraud, waste, and abuse.
Addressing the underlying issues in the PBM industry requires persistence and tenacity. Armed with proper knowledge, employers can begin asking their PBM the tough questions and start demanding more for their plan and for their members.
Schedule, engage, and pay your staff in one system with Workforce.com.
Recommended
Compliance
Minimum Wage by State (2024)federal law, minimum wage, pay rates, state law, wage law compliance
Staffing Management
4 proven steps for tackling employee absenteeismabsence management, Employee scheduling software, predictive scheduling, shift bid, shift swapping
Time and Attendance
8 proven ways to reduce overtime & labor costs (2023)labor costs, overtime, scheduling, time tracking, work hours